I had the opportunity this weekend to catch up on some of the presentations I missed at ATTD2024. I struck gold with the first one I watched. Dr Pratik Choudhary spoke on interpreting CGM data and, as I am in the process of building a bot to do this, it was a talk of great interest. The tips and tricks he gave for reading Ambulatory Glucose Profiles (AGPs) and the rest of the CGM report, I believe, are useful to anyone running a CGM.
Structural vs Behavioral Factors

Dr Choudhary considers two broad levers to improve what he sees in the data: Structural and Behavioral Factors.
For Structural Factors, Dr Choudhary applies general formulae to give a guide on what the values should tend towards if there is an issue.
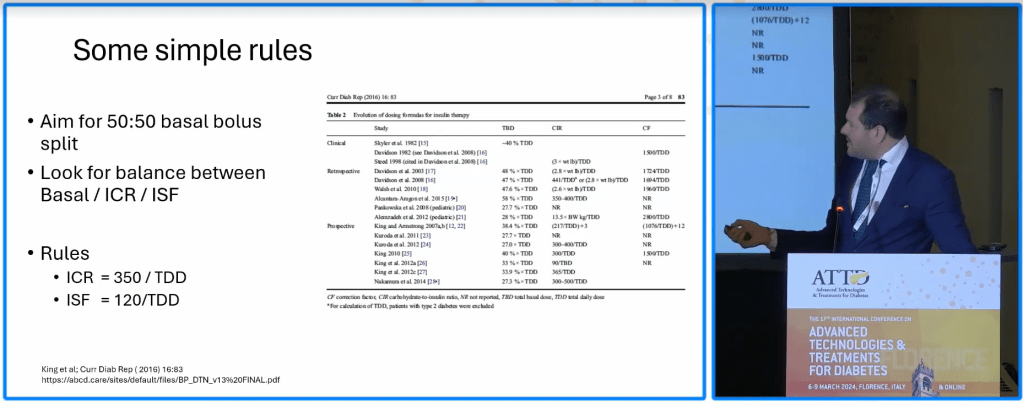
For people who bolus for meals, his general rules is a 50:50 split of daily units used for bolusing and daily units used for basal insulin. He mentioned exceptions to this rule such as low-carbers who will have a much higher percentage of basal and those who micro-manage their glucose levels, giving themselves boluses many times a day, who will have a higher bolus percentage. In these cases, if it is working, he leaves it alone but if it is not, the 50:50 rule is his guide.
For his benchmark carbohydrate ratio he uses 350 / Total Daily Dose and for the correction factor, 120 / Total Daily Dose.
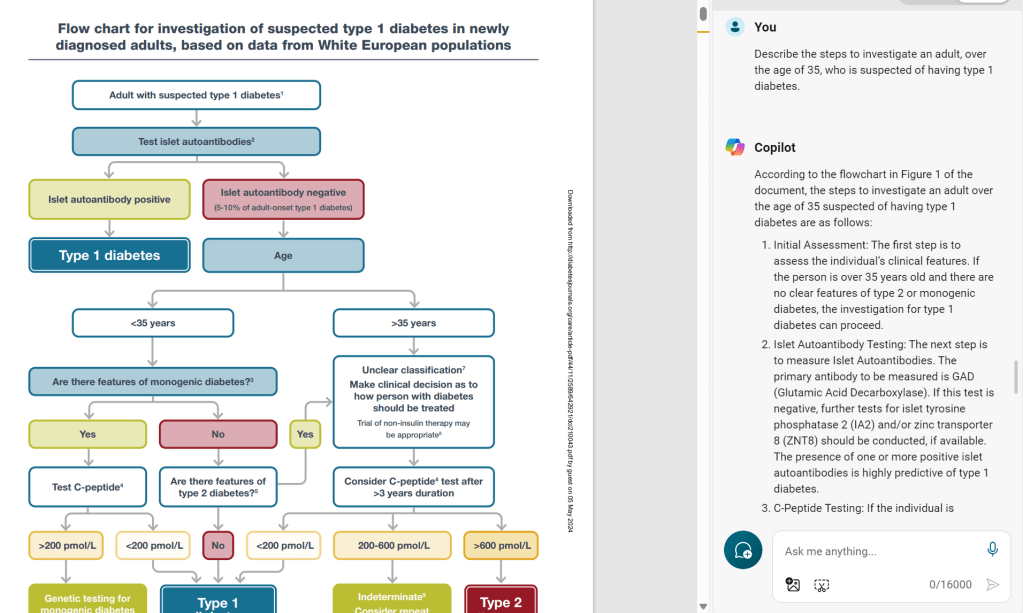
Dr Choudhary’s Flowchart

His position is, if the Bolus/Basal doses are as expected, the levers to pull are likely to be behavioral.

Showing an example, he presented a report for a person with diabetes (PWD) with top-heavy bolusing, based on the 50:50 rule. His experience is for top-heavy ratios, the PWD will often have a lot of variability. Considering the actual basal (32u/day) vs expected (39u/day) it suggests there is not enough basal, putting upward pressure on the CGM, rising between meals, which is confirmed in the graph.
The Insulin to Carb Ratio (ICR) was 5g/U whereas the predicted was 4.5 g/U suggesting a unit of insulin does not cover as much of a meal as the PWD thought. The Insulin Sensitivity Factor/Correction Factor was 2 mmol/L (1 unit of insulin drops blood glucose by 2mmol/L) whereas the predicted Correction Factor was 1.5 mmol/L suggesting insufficient insulin is being given corrections.
Sure enough, we see that the PWD is going high in the day and staying there, likely because they are not administering sufficient insulin due to bad factors/ratios, with the problem amplified by insufficient basal.
Behavioral Indicators

Dr Choudhary mentioned that for people without diabetes typical glucose variability is usually 15-20%. For PWDs between 20-35% they are generally looping or bolusing well. For people with a variability of 35-50% Dr Choudhary suggests this is a mismatch between food and bolus and so, in the case of high variability, he believes changing settings is not going to help. He also mentioned that any time a PWD can bolus 15 minutes before a meal is ‘free HbA1c/Time in Range and lower variability’.
The light blue area of the AGP relates to events which happen once every week or every fortnight, suggesting they are behavioral (or lifestyle driven e.g. an exercise day/Sunday roast/takeout night) more than systematic. Dark blue is more common and therefore more influenced by structural factors.
Where to Set the High Alarm
A great tip Dr Choudhary gave for setting the high alarm is at the top of the dark blue region on the AGP. When your blood sugar goes over this it is, by definition, an unusual event which may need intervention whereas anything below this is business as usual.
For low alarms, he warned setting them too high as it encourages the PWD to stay high, costing Time in Range. For myself, I set it to 3.3mmol/L (59mg/dL). For the five years post-diagnosis that I was insulin-independent, I wore a CGM and often dipped into the high 3s (high 60s) and got as low as 3.4mmol/L but never any lower. Therefore, below 3.4mmol/L, for me, is abnormal and worthy of attention.
Good Numbers but at What Cost?

Dr Choudhary also showed someone with excellent control due to frequent management. His recommendation for someone bolusing is to “scan, inject, eat and forget” meaning that once you have bolused and eaten, the trajectory of the blood glucose is set and there is very little which can change it. If the peak occurs around one hour after eating, you matched the bolus to the food. The level after two hours will indicate whether the bolus was enough to cover the food. After three hours may show rises influenced by protein and fats but he suggested there was little point in monitoring glucose movement around meals more frequently than this.
He also suggested that frequent management driven by fear of long-term complication may be ill-founded in some cases. From the DCCT study he cited that if a PWD has not had complication interventions in 20 years since diagnosis, their change of getting a life-changing complication for the rest of their life (loss of organ/sight/limb) is negligible. Therefore, if a person with this level of aggressive management is burning out after 20 years of micro-management the evidence supports the option of relaxing the regimen somewhat without significant consequence.
How Do I Fare?
As it happens I have just seen my Endo and my HbA1c has crept up to 5.9% so I am keen for suggestions on improvement (even though I am still well below the threshold for significant risk of complication ).
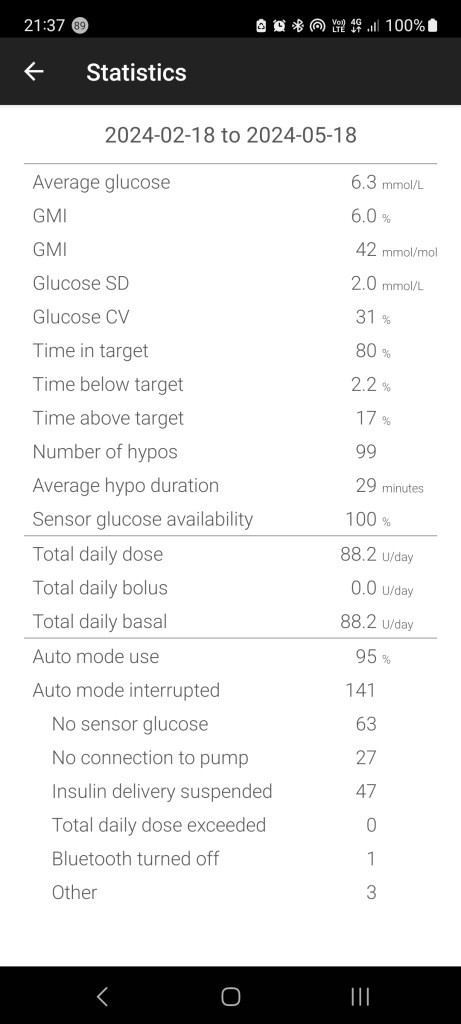
In terms of the structural settings, my Total Daily Dose for the last 3 months averaged 88U/day. However, as I run my CamAPS Ypsopump completely closed I do not bolus for meals and let the pump take care of it. Therefore, I cannot assess whether I am near the suggested 50:50 ratio. For 88U, the expected ICR is 4.0 g/U and the ISF is 1.4 mmol/L. Again, as CamAPS has automatically adjusted these values for me automatically as part of the loop I cannot check it directly but these values closely align to the default profile values in my pump which I determined using Android APS and Autotune, prior to switching to Ypso a couple of years ago.
My Glucose Variability is currently 31% which is in the typical range for someone looping but, as it is towards the higher end of the range suggests a slight mismatch between bolus and food. Given I let the algorithm do it all, this makes sense as I do not even declare I am eating, letting the loop figure it out for itself.
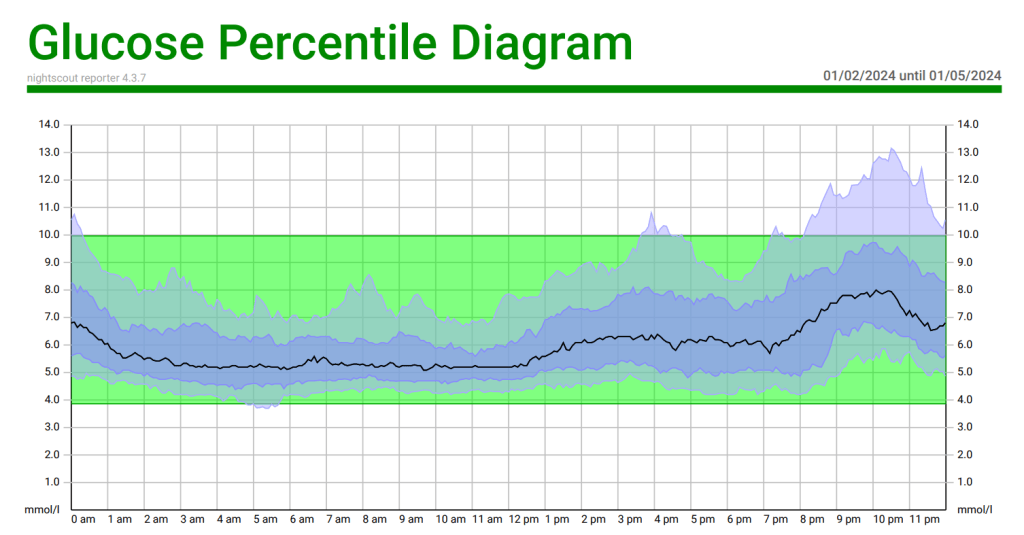
Looking at the dark blue, we can see a mismatch between insulin and dinner. As the family has roughly the same dinner on a given night of the week it would be interesting to see if the light blue is caused by “Lomo Saltado Lunes”, “Taco Tuesday”, or “Takeout Friday”. I will have to see if it is possible to generate AGPs for a given day of the week over a period on Nightscout…
My Endo has suggested providing some intervention to help the loop with dinner. CamAPS has a Boost function which I will activate at the start of dinner for two hours, giving the loop permission to be more aggressive, to see if this helps. Failing this there are plenty more levers to pull (restricting carb intake or, heaven forbid, giving a bolus).
As mentioned, my low alarm is set to 3.3mmol/L. You will see in the above stats that in the last 3 months it recorded 99 hypo values. These are, almost without exception, a new G6 sensor needing calibration. On the rare occasion I skip a meal and confuse the loop, I might skim the low alarm but it is nothing a few jelly beans cannot fix.
At the moment, my high alarm is set to 15 mmol/L (270mg/dL) but, based on Dr Choudhary’s advice, it should probably come down to 10mmil/L (180 mg/dL) if I was planning to intervene (at this stage I do not do correction doses either).