I just put together a Sick Day Plan/Guide for my Family in Case I am unconscious. I thought I would share it so others can craft it to make it their own. The guidelines are taken from the Australia Diabetes Education Association (https://www.adea.com.au/wp-content/uploads/2020/09/Consumer_01_10.pdf)
I have written them for someone with a pump (because I have a pump) and while the administering of insulin can be done with a pump, in an emergency, I made the call that a family member would be more capable of injecting insulin than checking if a pump still had insulin and using it to give a bolus.
I am not a medical professional so I strongly recommend running your version of this plan past your health care team before using it.
The Template
Sick Day Plan
Contacts
| Relationship | Name | Contact Number |
| Partner | <Partner Name> | <Partner Phone Number> |
| Endocrinologist | <Endo Name> | <Endo Phone Number> |
| Diabetes Educator | <DE Name> | <DE Phone Number> |
| GP/Family Doctor | <GP Name> | <GP Phone Number> |
| Dentist | <Dentist Name> | <Dentist Phone Number> |
| Cardiologist | <Cardiologist Name> | <Cardiologist Phone Number> |
What To Do When Sick/Unconscious (Looping Insulin Pump Plan)
- FAMILIARISE YOURSELF WITH THE INSTRUCTIONS BEFORE ACTIONING THEM
- If feeling unwell, Leon is unconscious, or BGL > 15mmol/L (270mg/dL) for more than 2 hours
- Check Blood Glucose Levels (BGLs) and Ketone Levels
- Continue to drink (0.5-1 cup of fluid per hour) and eat if possible (15g carb per hour)
- If BGLs greater than 10mmol/L (180mg/dL)
- Low carb intake and use insulin (<Inset enough to get you down to, say, 4mmol/L (72mg/dL))
- If BGLs less than 4mmol/L (72mg/dL)
- Take fast acting carbs
- Check BGLs every 15 minutes and treat until above 4mmol/L (72mg/dL)
- If ketones 0.6 – 1.5mmol/L (60 – 150 mg/dL)
- Change pump site
- Check BGL/ketones every hour
- Give 20% of your Total Daily Dose (TDD) of insulin every two hours.
- If ketones >1.5mmol/L (150mg/dL)
- Give 30% of your TDD every two hours
- Otherwise
- Check BGL/ketones every 2 hours
- If vomiting stop taking Metformin and SGLT2i’s
NB: Plan may need adjustment if not running a looping pump.
Liquids With Carbs
- Fruit juice (10g/100mL)
- Tea with sugar (5g/teaspoon)
- Milk (5g/100mL)
Liquids Without Carbs
- Water
- Diet coke/pepsi
- Diet cordial
- Stock
- Tea without milk and sugar
When To Seek Medical Attention
- Leon is unconscious
- Blood Glucose Levels over 15mmol/L (270mg/dL) and not coming down after two insulin treatments
- Ketone levels above 1.5mmol/L (150mg/dL) and not coming down after two insulin treatments
- Low BGLs (<4mmol/L (72mg/dL)) even after two hypo treatments
- Persistent vomiting (>4 hours) or stained with red/green/yellow
- Cannot follow sick day action plan
- DKA symptoms
- Nausea/Vomiting/Stomach Pain
- Increased thirst
- Increased urination
- Rapid, short breathing
- Fruity smelling breath
- Drowsy, weak, or confused
- Rapid heartrate
- Headache
- Blurred vision
- Dry skin
Note: Leon should not drive if he needs medical attention
How to Test Blood Sugar Levels
- FAMILIARISE YOURSELF WITH THE INSTRUCTIONS BEFORE ACTIONING THEM
- Get the black diabetes kit (usually in the blue diabetes bag in the craft cupboard)

- Take out the Genteel lancing device, Test Strip container (remove a test strip), and the Glucometer
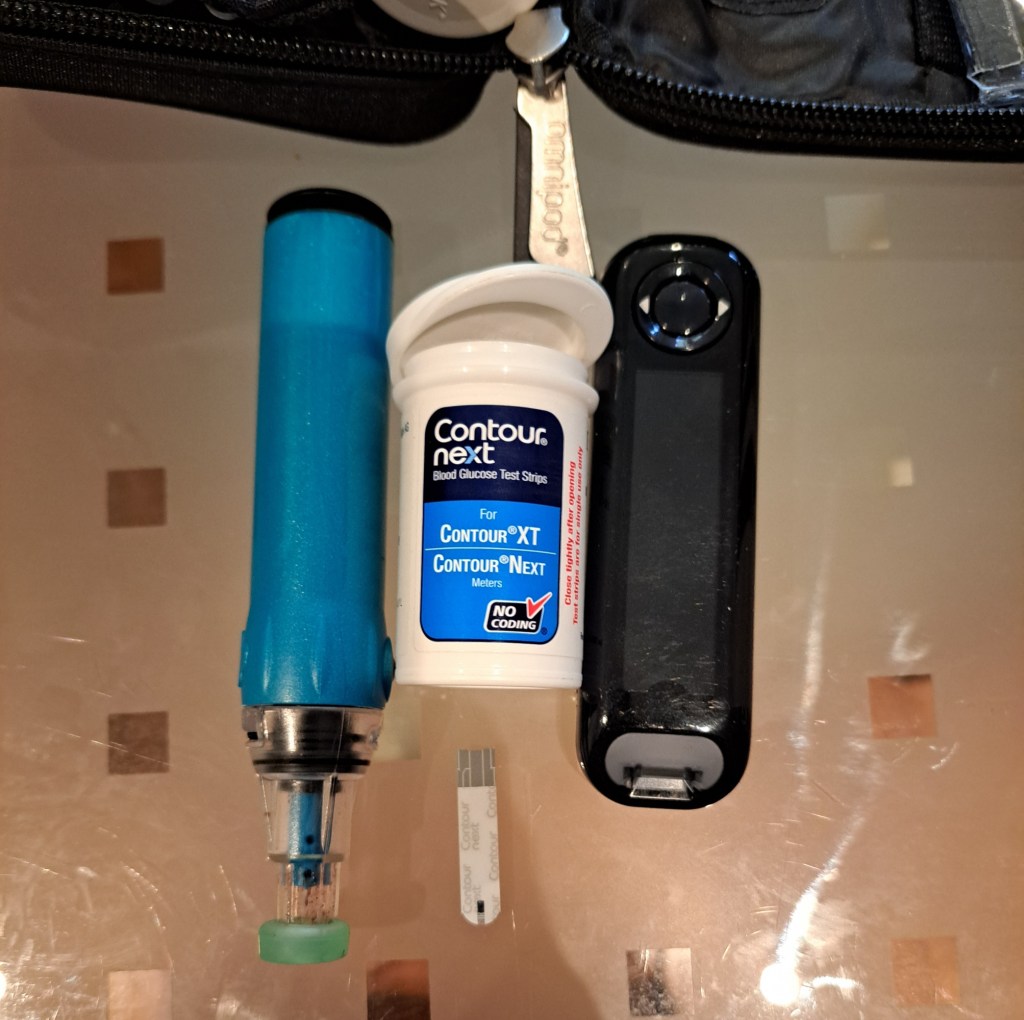
- Place the grey end of the test strip into the glucometer where the slot is
- Place the Genteel against a finger tip
- Press and hold the black button. You should see blood appear at the site in contact with the fingertip
- If you fail to draw blood push the plunger back down until it clicks and try again
- Dip the inserted test strip into the blood until the glucometer beeps
- Wait a few seconds and it will tell you Leon’s blood glucose level
How to Test for Ketones
- FAMILIARISE YOURSELF WITH THE INSTRUCTIONS BEFORE ACTIONING THEM
- Get the black diabetes kit (usually in the blue diabetes bag in the craft cupboard)

- Take out the Genteel lancing device, a Purple Test Strip in foil, and the Ketone Glucometer

- Place the black striped end of the test strip into the glucometer where the slot is
- Place the Genteel against a finger tip
- Press and hold the black button. You should see blood appear at the site in contact with the fingertip
- If you fail to draw blood push the plunger back down until it clicks and try again
- Dip the inserted test strip into the blood until the glucometer beeps
- Wait 10 seconds and it will tell you Leon’s blood ketone level
How to Give a Glucagon Injection
Only to be done if the blood sugar levels are less than 3mmol/L (52mmol/L) and unresponsive/unable to eat/drink.
NB: I could find no good guidance on when to use glucagon other than ‘when low’ so feel free to adjust the 3mmol/L level to one which works for you and your health care team.
The glucagon kit can be found in the blue diabetes bag in the craft cupboard in the front pouch.
Watch the video “How to do a glucagon injection” video on YouTube by University College London Hospitals NHS Foundation Trust (https://www.youtube.com/watch?v=9dDJQPHJq3w)
How to Inject Insulin when Leon is High (>15mmol/L (270m/dL))
- FAMILIARISE YOURSELF WITH THE INSTRUCTIONS BEFORE ACTIONING THEM
- Get an orange injection pen from the fridge (butter compartment or the grey cooler bag)
- Get a needle from the fridge (butter compartment)
- Remove paper cover from bottom of needle
- Remove top from insulin pen
- Screw the needle onto the insulin pen and remove the two needle caps
- Dial 1 unit and press the dialler down until you see insulin come out of the needle
- Dial the units indicated above
- Push the needle into a fatty area of the body e.g. belly
- Press the button down and leave it in while you count to 10
- Remove the injection pen from the injection site and cover the insulin pen with the pen’s blue cap to hide the needle tip