Michelle Law has an excellent blog over at Pumps and Pricks. One thing she does is a ‘Top Ten’ of the conferences she attends. This year, like me, she attended EASD 2023, thanks to Dedoc, and posted her Top Ten Highlights. I have purposely not read it because this blog will do the same for EASD 2023 and ISPAD 2023. It will be interesting to see the areas of research that spoke to both of us and our different takes on them. The ranking of ten to one is not important; they are all interesting announcements/areas fo research.
10. Type 1 Diabetes Before Insulin
With drugs like Teplizumab which can delay the progression of type 1 diabetes, research is now focusing on the disease before the person becomes insulin dependent. These days there are four stages for type 1 diabetes with insulin only being needed in the third stage.
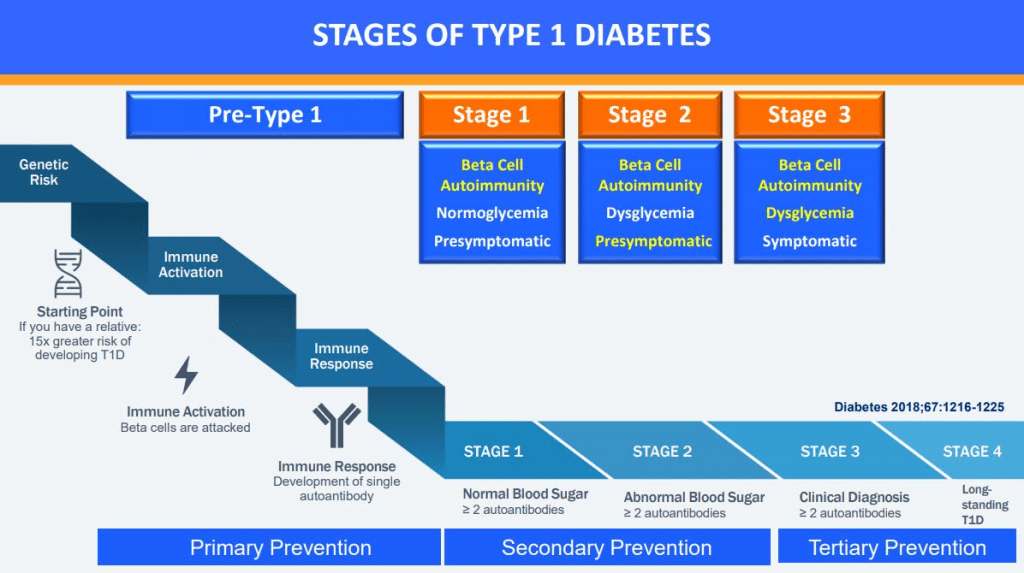
How do we know someone is likely to develop stage 3 type 1 diabetes? Because of the auto-antibodies in their blood which appear years before insulin is needed.
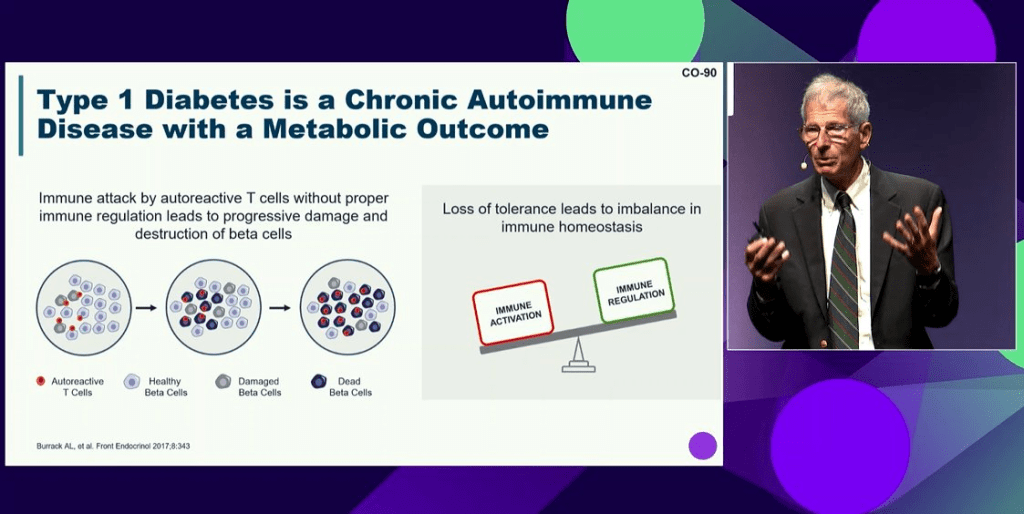
To shift this paradigm of type 1 diabetes being ‘insulin-dependent diabetes’, Kevan Herold described type 1 diabetes as an autoimmune disease with a metabolic outcome i.e. the beta cells stop working.
Flemming Pociot spoke of the limitations of just relying on auto-immune markers for early detection and how improved detection could be achieved by looking at genetic information and lipid profiles (FDR = First Degree Relative e.g. parent).

9. Time in Range is the New HbA1c
While there are plenty of people in the world without access to Continuous Glucose Monitors (CGMs), the people of Europe are generally not those people. So, it makes sense that the conferences focused a lot more on Time in Range (TIR) than on HbA1c.
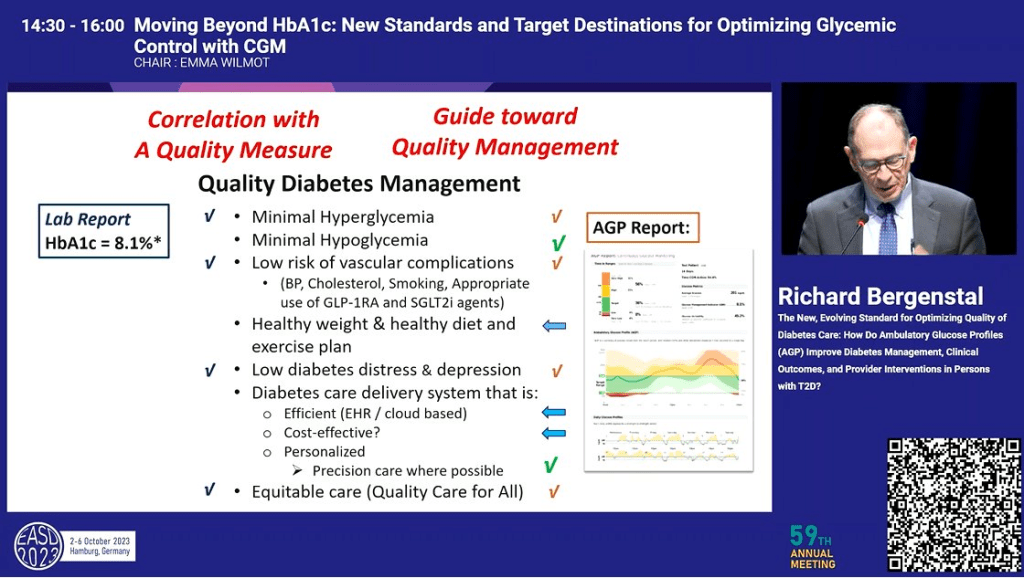
Richard Bergenstal showed that, from a research perspective, TIR is as predictive as HbA1c
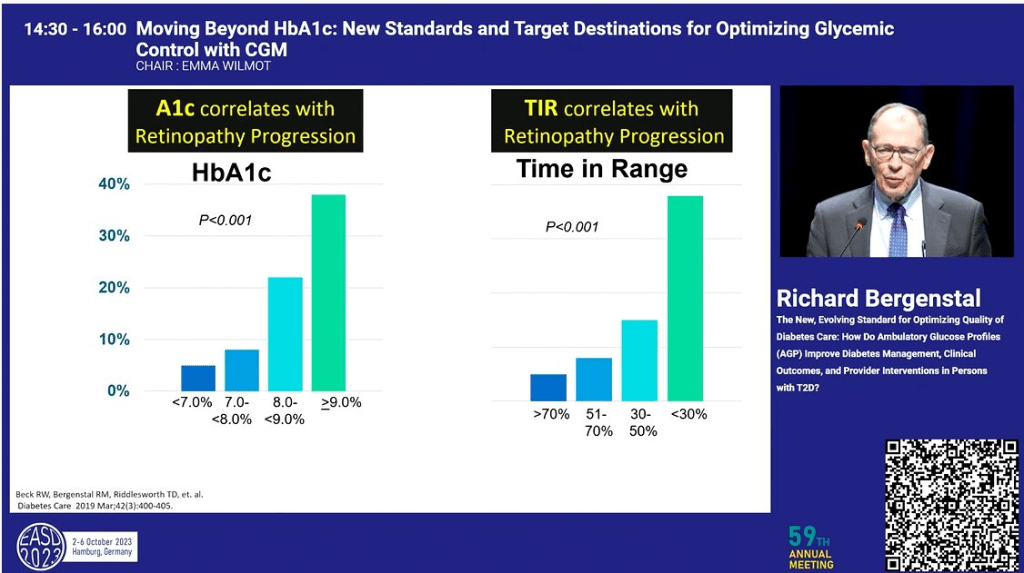
and provides a wealth of information an HbA1c measure does not, providing better guidance for the management plan for the disease.
Throughout the two conferences, as touched on below, many of the outcomes were focussed on Time in Rage, Time Above/Below range rather than HbA1c.
8. Exercise and Diabetes
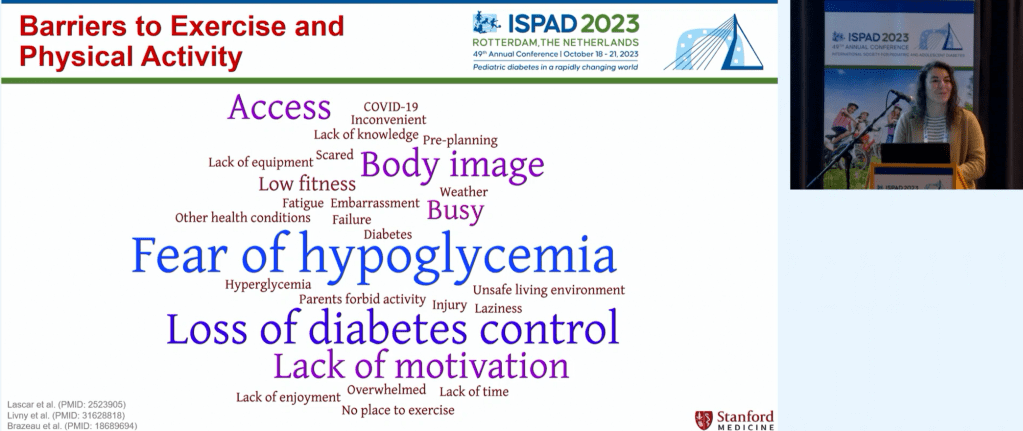
There was a lot of talk about exercise at the conferences. Dessi Zaharieva spoke of the known benefits of exercise for people with diabetes.

and the barriers people with type 1 diabetes often face when considering exercise.
John Pemberton showed a post-meal walk can have a significant, positive impact on glucose levels.

Jennifer Leohr showed Lyumjev (URLi) worked better with exercise than Humalog (Lispro) inducing less hypos.

7. Looping/Automated Insulin Delivery (AID)
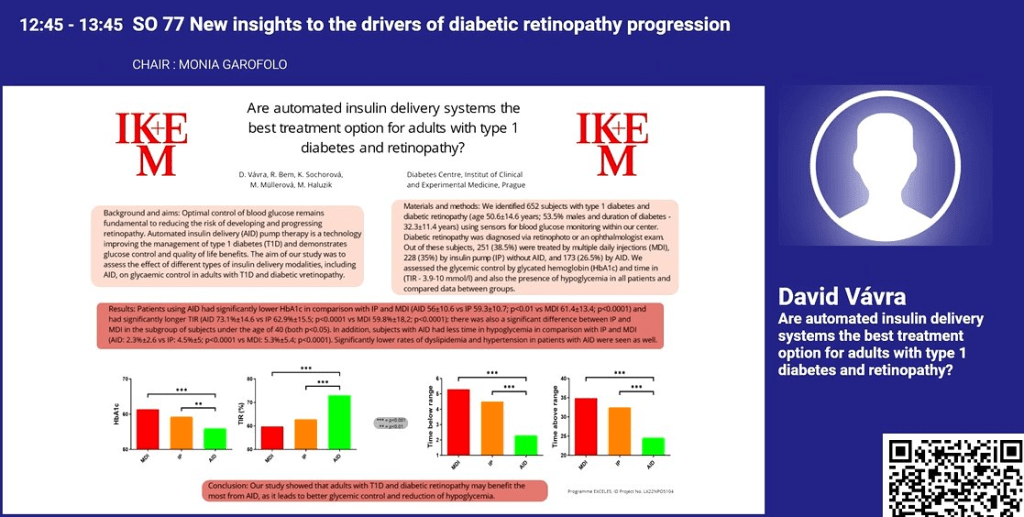
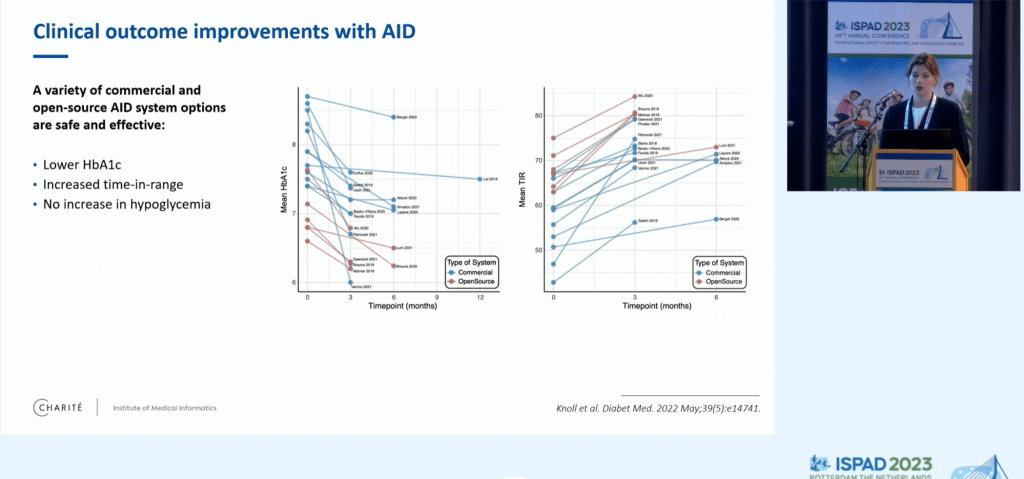
As we have seen in previous conferences, Looping systems (AID) showed superior performance to insulin pumps (IP) and multiple daily injections (MDI).

David Vavra showed similar results for HbA1c as well as other measures.
Javier Castaneda showed how 82% of those using the recommended settings on the commercial Minimed looping system achieve a Time in Tight Range (TITR) of over 50% which is, according to Thomas Danne, is sufficient to avoid long-term complications.

Comparing open-source looping systems to the commercial ones, Ludek Horvath found the open-source system yielded superior results but this could be a function of the people using them rather than any inherent advantage.
He also showed that looping systems achieve greater than 70% time in range which is significantly larger, and more consistent across countries, than the use of non-looping pumps or injections.


Katarina Braune also confirmed that open-source systems are at least as good as the commercial ones.
Yves Reznik talked about a study looking at people with type 2 diabetes, insulin dependent, but unable to give themselves injections. Moving to a looping system significantly improved their blood glucose levels.

At ISPAD, Roman Hovorka spoke of what is desirable in a looping system and confirmed “The right system is the one people are willing to use”.
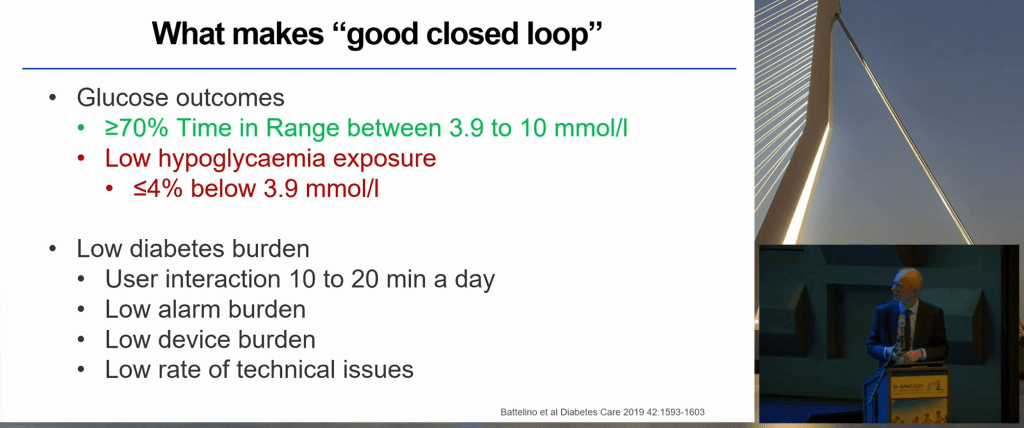
There was also increased talk of ‘fully closed looping’ i.e. no manual bolusing or declaration of meals which I had not seen much of in previous conferences. Sarah Koning looked at how many grams of carbohydrate a loop can tolerate in a meal without announcements. The answer is somewhere between 0-60 and at least 20g. While meals of 61-80g led to less Time in Range (TIR) and Time Above Range (TAR) with fully closed looping, there was no increase in hypos or DKAs.

Lenka Drnkova (Petruzelkova) showed that a fully closed open-source loop performs as well as the same system with manual boluses or no-bolus meal declarations. There are still some kinks to work out though e.g. exercise.

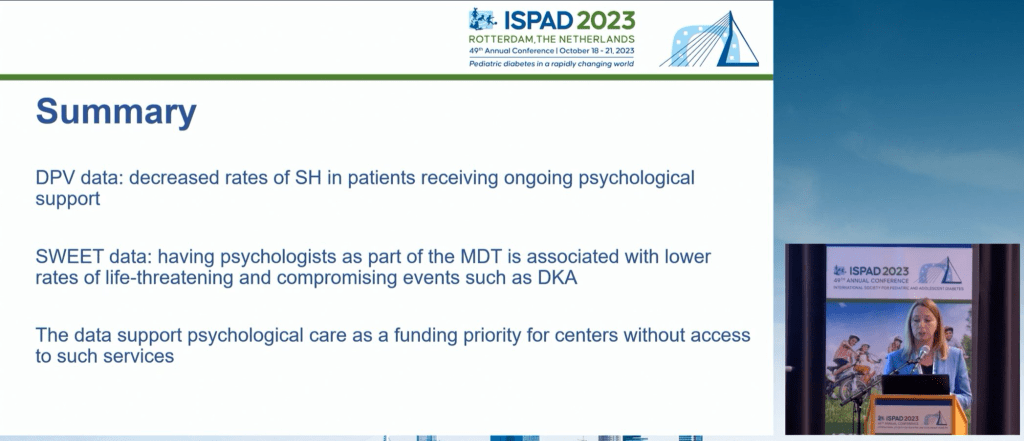
6. A Psychologist as Part of the Diabetes Health Care Team
There was a lot of talk of a mental health specialist being part of the person with diabetes’ health care team. Agnieszka Szadkowska summed it up nicely in this slide where the psychologist is on equal footing with the rest of the therapeutic team.
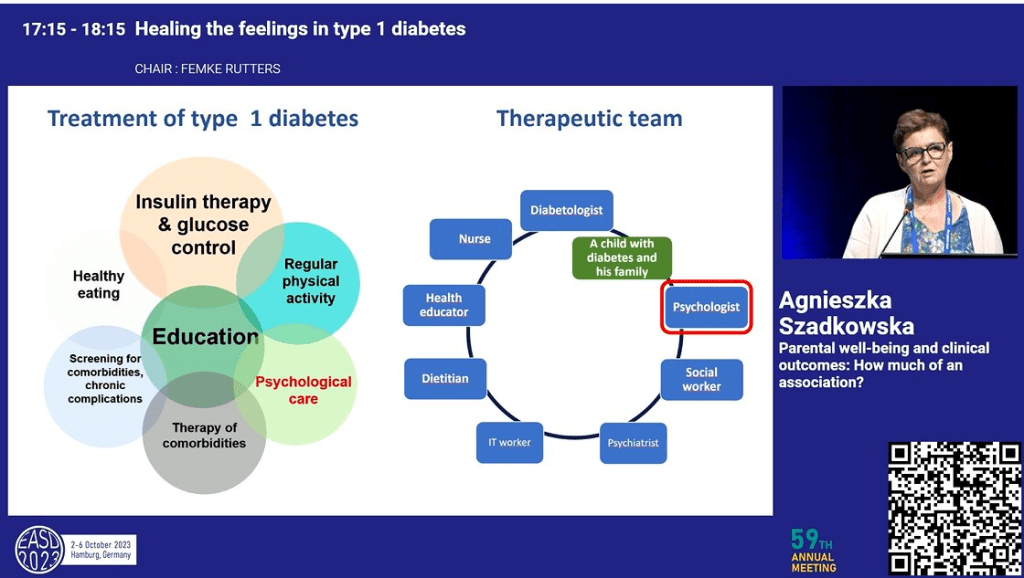
Evelyn Cox presented preliminary findings linking mental health management with better clinical outcomes e.g. HbA1c and Time in Range.

Agata Chobot linked on-going psychological support for people with type 1 diabetes with improvement in severe hypoglycemia and DKA rates.
5. End Diabetes Stigma
The recognition of the end diabetes stigma campaign was throughout EASD 2023, starting out with the presidential address.
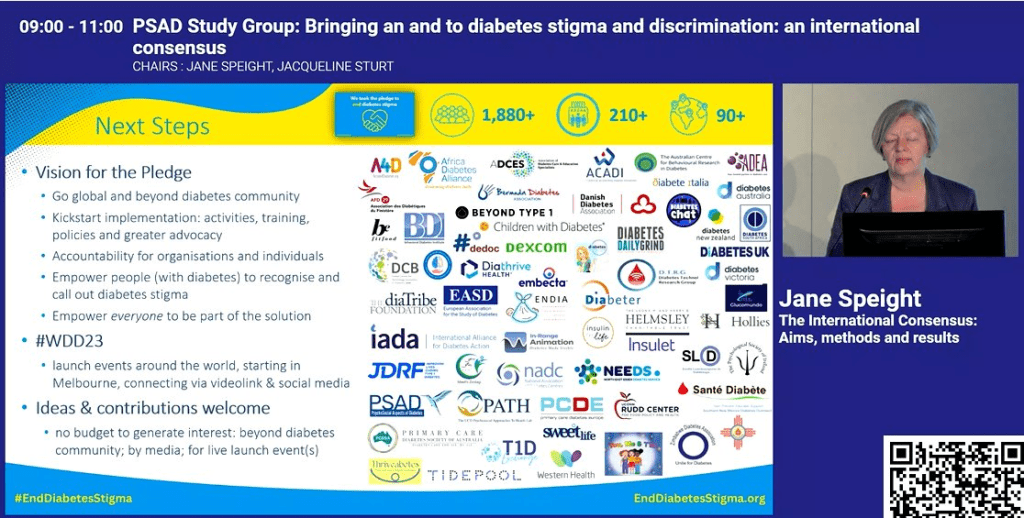
Jane Speight talked about those behind the campaign, how the pledge was created

and expanded on how many individuals and organisations had signed, and the reach of the campaign so far.
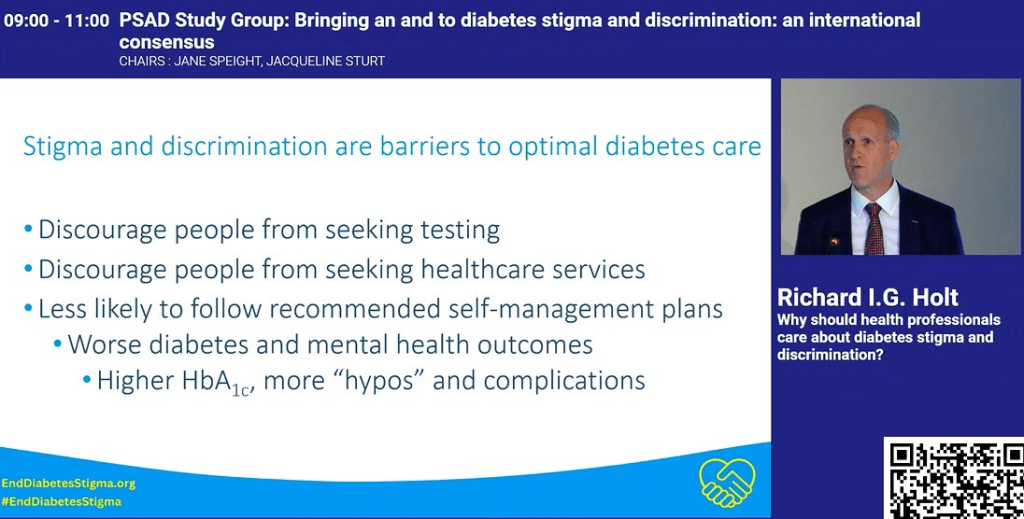
Richard I. G. Holt provided examples of how healthcare professional can be unwittingly part of the problem

and how stigma hinders optimal care.
4. Dual/Triple Agonists
Incretin Mimetics such as Ozempic/Wegovy have been big news for a while because, as well as being an excellent medication for type 2 diabetes, can result in weight loss. The next generation of these drugs are now coming to market and, while drugs like Ozempic target one type of receptor in the body, these new versions target 2 or more.
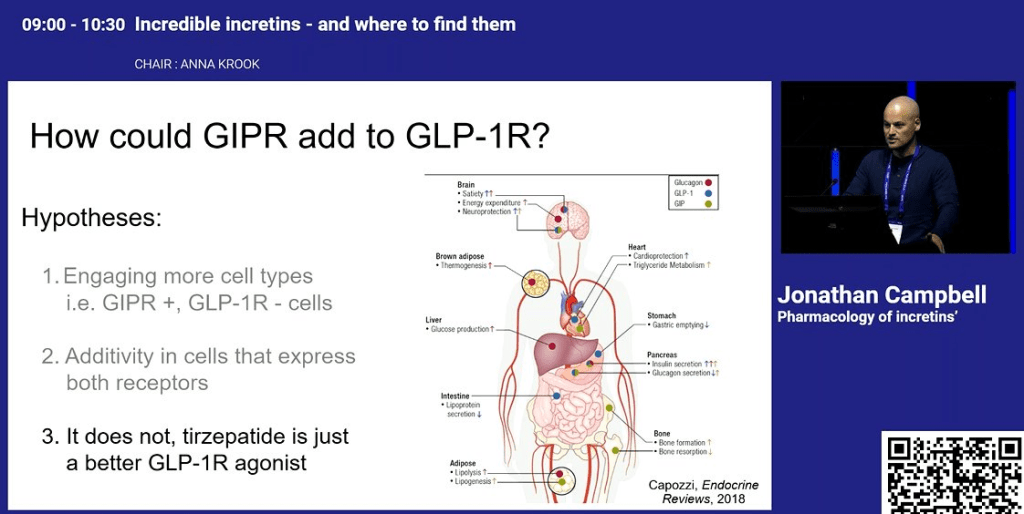
Jonathan Campbell talked about how dual agonists such as Tirzepatide work and, while they know what they do, how they do it is not as clear.
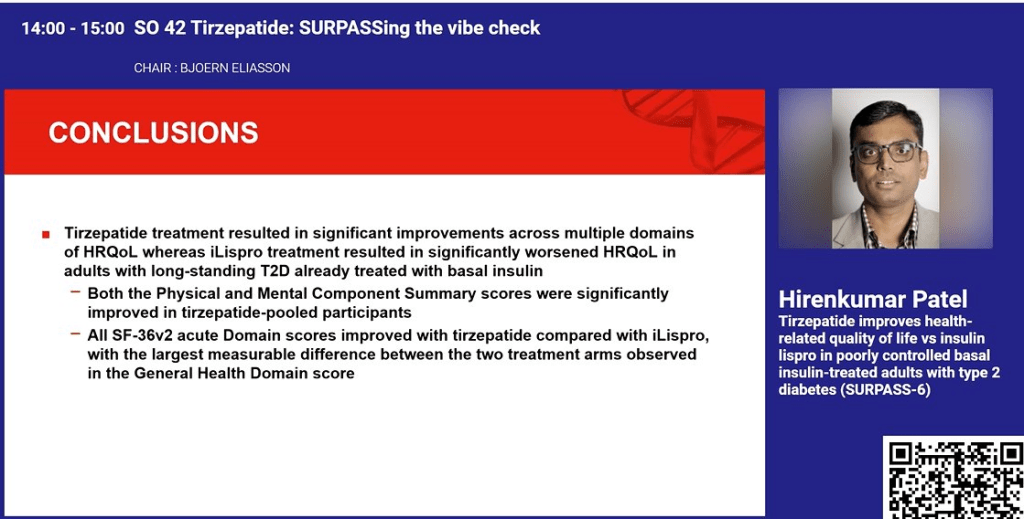
Hirenkumar Patel showed that, for people with type 2 diabetes, the use of Tirzepatide gave better results, both qualitatively and quantitatively, than basal insulin injections.
Eda Cengiz spoke of new research in a triple agonist which led to a 2% drop in HbA1c.

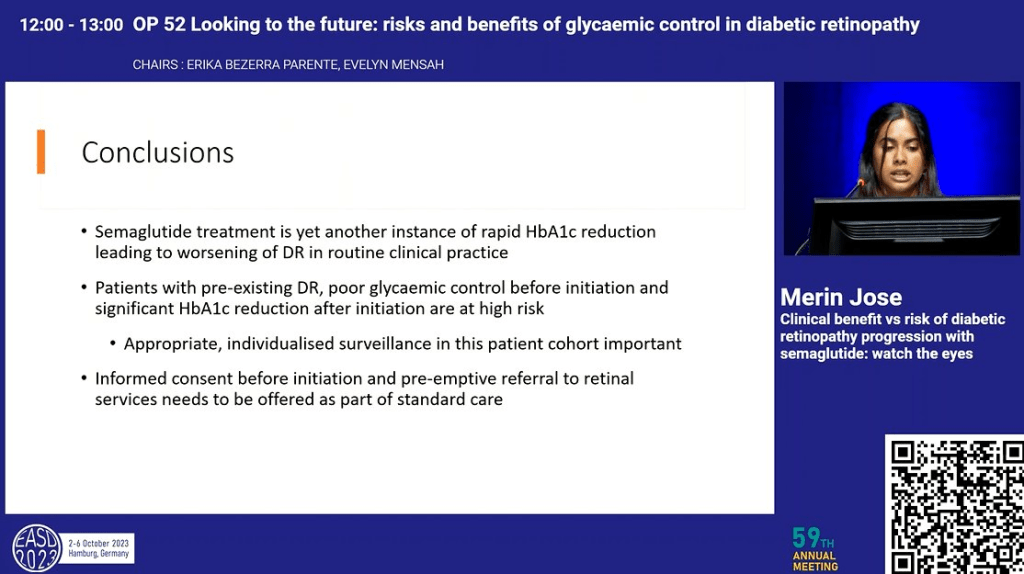
Merin Jose gave a word of warning that the rapid reduction in HbA1c resulting from these drugs can increase of the risk of diabetic retinopathy and this should be monitored closely.
3. Sleep and Diabetes
The benefits of sleep for people with diabetes came up during the conferences. Natalia Marhefkova showed how good sleep patterns directly affect outcomes e.g. a lower HbA1c. When asked by the audience what the ideal amount of sleep was, Natalia claimed it was 7-8 hours.

Erin Cobry also touched on the benefits of sleep for people with type 1 diabetes.
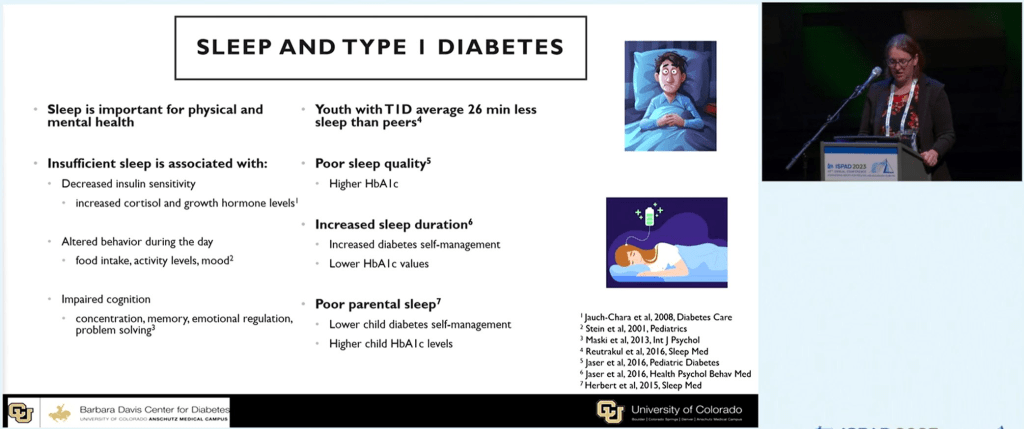
She also went on to talk about how Looping (AID) facilitates uninterrupted sleep and how even the interrupted sleep of carers can affect the clinical outcomes of the child they care for.

2. Diabetes and Diet
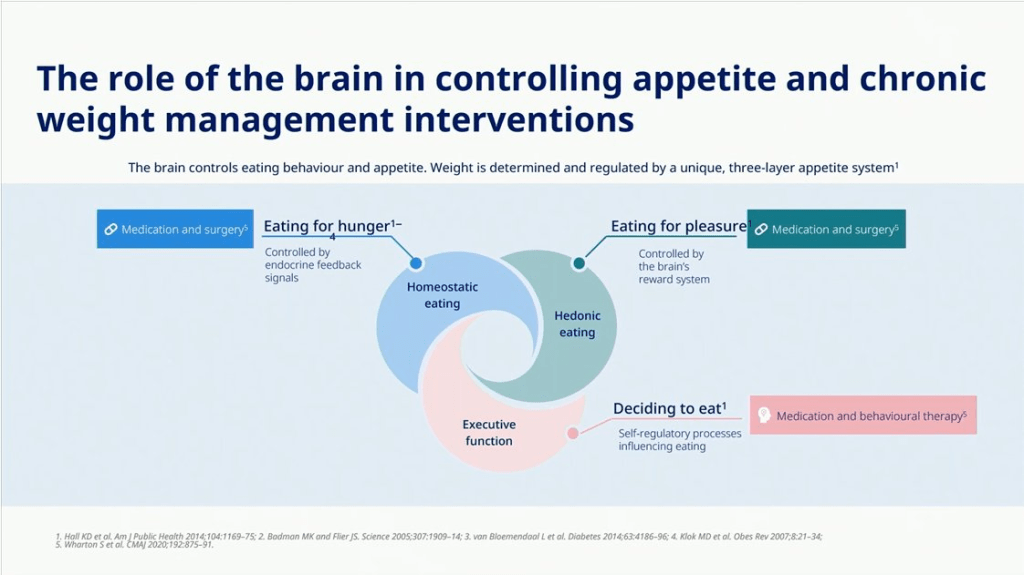
Jens Aberle talked about how if we plan to help manage the diet of people with diabetes, we need to better understand the reasons people are eating.
Emma Wilmot talked of a study which had confirmed that eating the carbohydrate foods last in a meal can have a significant impact on glucose peaks.

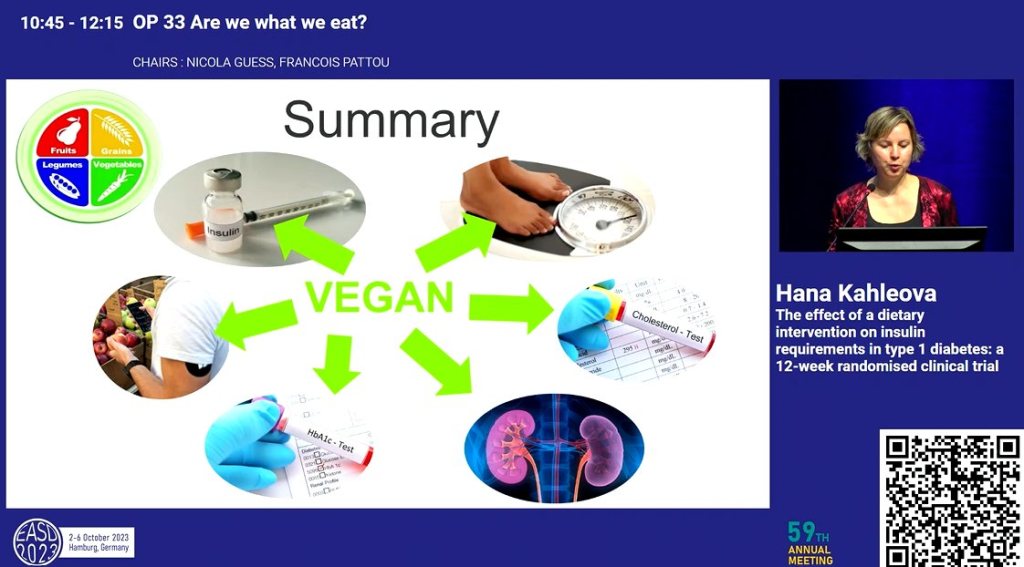
Hana Kahleova presented a study comparing a vegan diet to the ‘healthy plate’ and found while the healthy plate provided benefit in Hba1c and cholesterol, the vegan diet saw benefit in these and other measures such as daily insulin need, which was reduced, despite an increase in carbohydrate in-take.
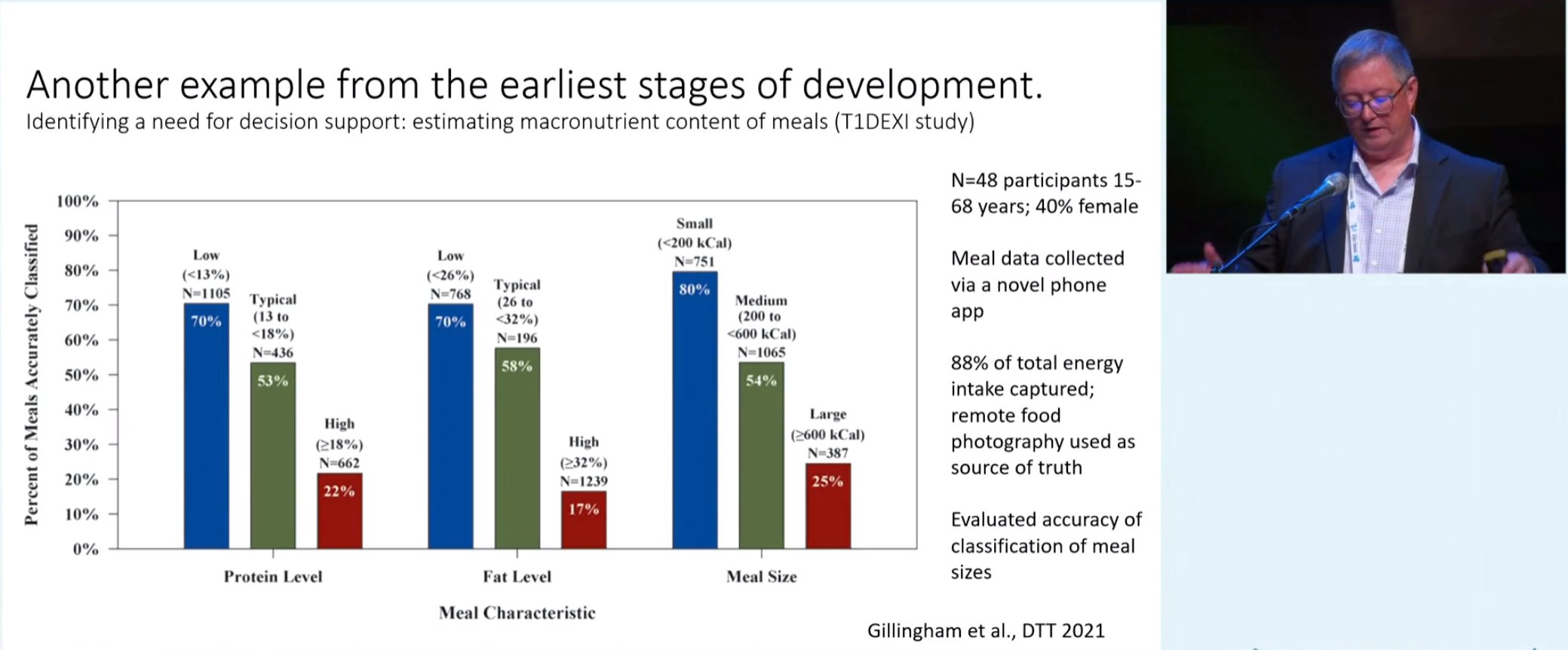
Mark Clements talked about how smaller meals are easier to estimate for their carbohydrate content than larger ones
and how people with diabetes tend to underestimate the carbohydrate content of larger meals.

1. SGLT2is
This class of drugs lowers the threshold at which the body redirects blood glucose to the bladder. Aikaterini Eleftheriadou spoke of the benefits of SGLT2is compared to incretin mimetics in regard to long term complications.

Aino Latva-Rasku showed SGLT2is increase skeletal muscle and brain uptake in fatty acids in people with type 2 diabetes. One explanation is SGLT2is change the body’s preference for fuel source.

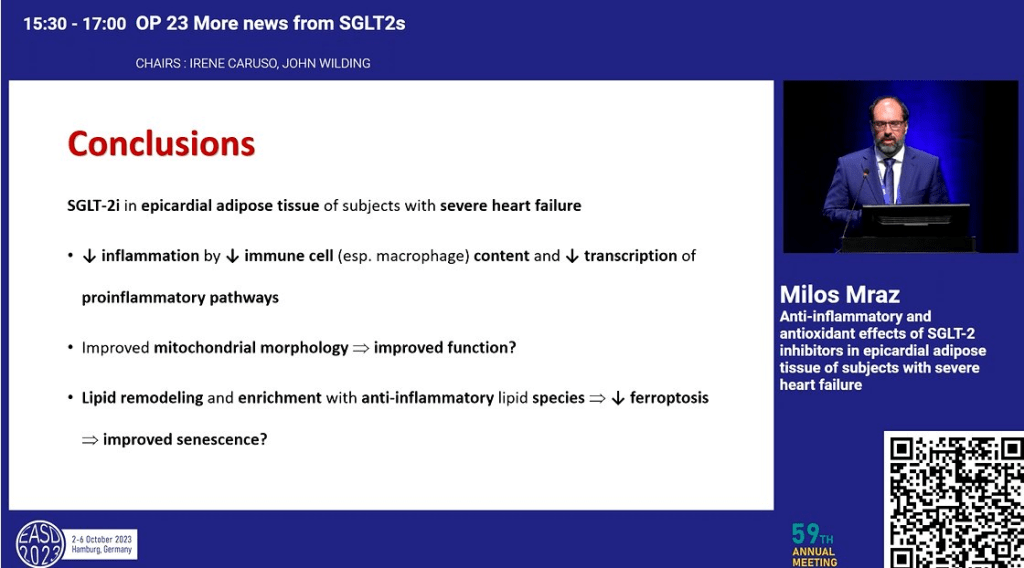
Milos Mraz spoke of the anti-inflammatory benefits for Type 1 Diabetes and while the blood glucose redirection mechanisms are understood, the other effects observed are not quite yet understood, similar to incretins.
Conclusions
My final thoughts (thanks Michelle) are:
(10) Type 1 Diabetes Before Insulin: The expansion of type 1 diabetes to consider the time ‘before insulin’ e.g. Stage 1 and 2 is really interesting. I wonder if this will lead to reclassification of LADA as simply a slow progressing form of Stage 2, Type 1 Diabetes.
The progress of early intervention type 1 drugs, such as Teplizumab, is really exciting and, hopefully will lead to a cure. One presentation spoke of using a combination of drugs whose effect for slowing progression will be additive and potentially ‘cure’ someone of type 1 diabetes, with the person taking pills rather than injections. While it has been promised for decades, with looping technology and immune system modifying drugs, we are genuinely getting closer to a practical cure.
(9) Time in Range is the New HbA1c: There is clearly an increased interest in using Time in Range (TIR) in academia, instead of the traditional HbA1c. My speculation as to “why?” is because it allows multiple secondary endpoints (additional measures) off of the same data whereas there is only so much you can do with an HbA1c measure. Unfortunately, bodies like the FDA who approve medications and diabetes technology still emphasize the value of HbA1c over TIR. This means for research to be useful to the manufacturers of the medications and technology, who also, in part, fund the research, HbA1c often needs to be the primary measure. Hopefully, in time, bodies like the FDA will see the value of TIR as a ‘primary endpoint’ in research.
(8) Exercise and Diabetes: There is increasing research into how to incorporate exercise into the lives of people with type 1 diabetes while allaying fears of hypoglycemia. This is great and can only be a good thing for diabetes management. For years I avoided exercise because of the concern of the effect it may have on short term blood glucose levels. Using the research, I am seeing at these conferences, I am now putting together a program for myself, and hopefully others with type 1 diabetes, which will help them introduce exercise into their lives safely.
(7) Looping/Automated Insulin Delivery (AID): Looping goes from strength to strength and there is a genuine belief in the looping research community that we are close to a fully closed loop. From my own experience I know of how looping reduces the burden of diabetes management significantly. While not a cure per se, looping makes mental room for other aspects of life and, for many, will bring precious relief from the constant harassment of management.
(6) A Psychologist as Part of the Diabetes Health Care Team: The rise in prominence of a psychologist on the health care team is well overdue and I look forward to this academic acknowledgement move to government policy and subsidised consults. While not disputed, the mental burden of diabetes management is rarely openly acknowledged. Access to psychological services, as a given for diabetes management, would be a huge step in this regard.
(5) End Diabetes Stigma: The rapid rise of the End Diabetes Stigma campaign is interesting. I have signed the petition and I hope it leads to something tangible for people with diabetes. People hide the fact they have diabetes and do not seek the help they need out of misplaced shame and embarrassment. This, in turn, leads to poor outcomes. In this sense ending diabetes stigma will save lives and improve the quality of life for many.
(4) Dual/Triple Agonists: This class of drugs is providing substantial benefit to people with diabetes, and I have spoken of these benefits in the past. In moving to double and triple agonists we are seeing an amplification of the effect and benefits and, while we do not completely understand the mechanisms in play, the promise of these drugs is significant.
(3) Sleep and Diabetes: For type 1 diabetes, interrupted sleep was often inevitable because of highs and lows, or because of split basal dosing. In the case of carers, the monitoring of the child with diabetes through the night also guaranteed broken sleep. Automated alarms and looping open the door for a complete night’s sleep for all. For myself, thanks to looping, a broken sleep because of diabetes may happen once a month but little more. Now I just need to work on getting the 7-8 hours sleep a night suggested to be optimal…
(2) Diabetes and Diet: While social media is awash in food hacks for people with diabetes, it is still good to have research-backed evidence on what is proven effective. Whether it is considering the psychological aspects of eating, or the practicality of estimating carbohydrates in a large meal, all of this informs people with diabetes on the best approach for them which has the best probability of success.
(1) SGLT2is: While there is still work to go on making these generally available for people with type 1 diabetes, due to factors such as the increased risk of DKA and eDKA, it is clear there are tremendous benefits in using them. I use a low dose SGLT2i at the moment, in combination with exercise once per week, and have seen a literally halving in my daily insulin needs and, without altering my diet, rarely see excursions beyond 8 mmol/L (144 mg/dL).
Thank you again to Dedoc for making it possible for me to attend these conferences and I strongly recommend, if you are an advocate who can #PayItForward to your community, applying for a Dedoc scholarship to attend a conference in 2024.